Accuracy of the Ovulon Fertility Monitor to Predict and Detect Ovulation
Abstract: The purpose of this pilot study was to correlate the three biologic markers of the Ovulon fertility monitor (a long-term predictive peak about 6 days before ovulation, a short-term predictive peak about 1 day before ovulation, and a nadir at the time of ovulation) with the peak in cervical mucus and the luteinizing hormone (LH) surge in the urine. Ten volunteer subjects (mean age 30.2 years) monitored their cervical-vaginal mucus, the surge of LH in the urine with a home assay test, and their vaginal electrical readings (with Ovulon monitors) on a daily basis for one to four menstrual cycles. In 19 of the 21 cycles that indicated a LH surge, there was a strong positive correlation between the LH surge and the peak of cervical-vaginal mucus (r = 0.96, P <= .01), and between the LH surge and both the Ovulon nadir and Ovulon short-term predictive peak (r = 0.84, P <= .01), and a modest positive correlation between the long-term Ovulon predictive peak and the LH surge (r = 0.62, P <= .01). The time of optimal fertility as determined by the peak in cervical mucus, the LH surge, and the Ovulon was similar. The Ovulon has potential as a reusable device to help women determine their fertile period.
The ability to predict and detect ovulation is critical for women who wish to achieve or avoid pregnancy. The most common methods of predicting ovulation in use today are monitored basal body temperature (BBT), self-observation of cervical-vaginal mucus, and self-testing of luteinizing hormone (LH) in the urine. All three of these methods have advantages and disadvantages. In recent years, a number of technological devices have been developed to help women determine their optimal time of fertility. This technology is important for women who are trying to achieve or avoid pregnancy. The devices include electronic and computerized BBT, hormonal test kits, cervical-vaginal fluid volume meters, and crystallization monitors (1).
A recently developed device to aid in the prediction and detection of ovulation is the Ovulon fertility monitor (Conception Technology Inc.; Fort Collins, CO). The Ovulon prototype consists of a hand-held digital monitor and a vaginal sensor that is inserted like a tampon, for about 30 seconds, on a daily basis (Figure 1). The vaginal sensor harmlessly detects bioelectrical measurements. The measurements are harmless because of two design features: 1) the biocompatible (carbonaceous) material of the active elements cannot release any harmful or potentially harmful substances into the vagina and 2) the electrical mode of measurement is such that no electrical energy is passed into the body and no electrochemical reactions (electrolysis) can occur.
The device is based on the changes in electrical admittance as a result of the sensitivity of the cervical tissues to steroid hormones such as preovulatory estrogen that stimulate the production of and changes in cervical epithelium and mucus. The electrical changes are theoretically produced by the oxidative-reduction reactions that take place in the mucus glycoproteins of the cervical mucus. The electron transfer reactions in the biologic material interact with the electronic structure of the active elements, and the interaction is detected by the measured admittance.
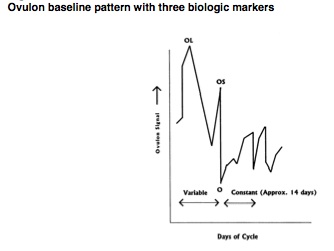
The OvuIon monitor can be used to both predict and confirm ovulation. The Ovulon monitor produces three biologic markers: a long-term predictive peak in electrical admittance about 5-7 days before ovulation, a second short-term peak about 1 day before ovulation, and a nadir of electrical admittance on the day of ovulation.
A device superficially similar to the Ovulon, the CUE fertility monitor, was developed by the Zetek Corporation (Aurora, CO) (2-4). Unlike the Ovulon, the CUE monitor uses both a salivary and vaginal sensor and is based on ionic conductivity as a result of aldosterone-stimulated concentrations of salt and water in the cervical mucus and saliva.
The Ovulon monitor has never been widely tested. Dr. Benedetto of the University of Torino Institute of Obstetrics and Gynecology tested an early model of the Ovulon with four young healthy women and reported in an unpublished study that they were all able to demonstrate a long-term predictive peak before the ovulation marker of the instrument and a short-term predictive peak about the day before ovulation, except for one case where a probable luteal phase defect was associated with the absence of the predictive peaks. Further study of the Ovulon monitor needs to take place to determine its applicability for family planning.
One method of determining the Ovulon's accuracy in detecting the fertile period is to compare it with other standard markers of ovulation. Two commonly accepted and researched methods of detecting ovulation are the self-observation of cervical-vaginal mucus and the self-detection of LH in the urine. The detection of LH in plasma or urine is considered by experts to be a standard method to predict ovulation (5,6). Manufacturers of ovulation tests kits claim a greater than 90% accuracy in detecting the urine LH surge, which occurs about 12-24 hours before ovulation (7,8). Optimal or "peak" cervical-vaginal mucus (defined as mucus that stretches 2.5 cm or more, is clear on appearance, and/or has the sensation of lubrication) as obtained from the vaginal opening also correlates closely with the day of ovulation and the day of the LH surge (9,10). The specific aim of this pilot study was to determine the accuracy of the Ovulon fertility monitor by comparing and correlating the peak in cervical mucus and the LH surge in the urine with the three biologic markers of the Ovulon monitor.
Methodology
Ten volunteer female subjects (mean age 30.2 years) with regular menstrual cycles (ie, cycles of 21-38 days in length) who were trained in the use of the Creighton model ovulation method of natural family planning (NFP) (mean months of use 32.0) monitored their cervical-vaginal mucus, the surge of LH in the urine with the OvuQuick assay test, and their vaginal electrical/chemical readings (with the Ovulon monitor) on a daily basis for one to four menstrual cycles using 10 prototype Ovulon monitors.
The LH surges in the urine were self-detected by use of the OvuQuick self-test kit. The OvuQuick is based on monoclonal enzyme immunoassay of LH in the urine. The test has a reported LH sensitivity of 30 mIU/mL. OvuQuick has shown a 98% agreement with other tests in detecting the LH surge (5).
The peak day of cervical mucus was determined by means of the Creighton model vaginal discharge recording system (VDRS), developed through research conducted at St. Louis and Creighton Universities over a 5-year period (11). The recording system requires that women check for cervical-vaginal mucus by wiping the outside of their vaginas (the vulvar area) every time they go to the bathroom to void and once before going to bed. The women check mucus for color, stretch, and consistency. The VDRS has a reported 99% method effectiveness and a 95% use-effectiveness for determining fertile and nonfertile days of the cycle (11,12).
An algorithm was developed to standardize the determination of the biologic markers of fertility asdetermined by the three methods, ie, the Ovulon monitor, the LH, and the cervical-vaginal mucus. The decision criteria for the Ovulon data are as follows:
- LH-the last day of the LH surge as detected in the urine with the home
- test kit and recorded on the fertility chart.
- P-the last day of mucus that was either clear on appearance, stretches an
- inch or more, and/or had the sensation of lubrication as observed by the
- subject and recorded on the fertility chart.
- OS-the day of the highest Ovulon reading. "OS" stands for the short-term Ovulon predictor (Figure 2).
- OL-the day of the highest Ovulon reading preceding the OS. OL stands
- for the long-term Ovulon predictor.
- O-the day of the lowest Ovulon reading after the OS.
Using the above algorithm, interrater reliability was determined between the decision of the principal researcher and a graduate student research assistant on the day of the observed biologic markers. The interrater ratio of the observed day of LH, P, 0, and OS was 100% and the OL day was 90%.
Results
Nineteen of the 21 menstrual cycles indicated an LH surge (Table 1). In the 19 cycles with an established LH surge, there was a strong positive correlation between the LH surge in the urine and the peak day of cervical mucus (r = 0.96, P <= .01), between the LH surge and the Ovulon nadir "O" (r = 0.84, P <= .01), and between the LH surge and the Ovulon short-term predictive peak "OS" (r = 0.84, P <= .01). There was a modest positive correlation between the long-term Ovulon predictive peak "OL" and the LH surge (r = 0.62, P <= .01). There also was a strong positive correlation between the peak day of cervical mucus and the Ovulon nadir (r = 0.86, P <= .01). In the 19 cycles in which an LH surge was detected, the Ovulon short-term predictive peak was within 3 days of the LH surge.
Discussion
Although the Ovulon monitor is based on a different technology than the CUE fertility monitor, the results of this study are similar to the strong correlation between the LH surge and the predicted day of ovulation (r = 0.79) found by Moreno et al. (4). The Ovulon's predicted day of ovulation "O" correlated positively with the LH surge (r = 0.84) and the peak in cervical mucus (r = 0.82). The conclusion, therefore, is that the Ovulon monitor has similar accuracy in predicting ovulation as the ovulation method of NFP, the urine LH detection kits, and the CUE fertility monitor. The short-term Ovulon ovulation predictor also had a strong correlation with the LH surge (r = 0.84) and the peak in cervical mucus (r = 0.86). The Ovulon short-term predictor ranged from 1 to 4 days with an average of 2.3 days before the Ovulon nadir. This short-term predictive peak would be especially beneficial for those women and couples trying to achieve pregnancy because fertility drops dramatically shortly after ovulation (13). The short-term predictive peak would not give enough warning time for those wishing to avoid pregnancy.
The long-term Ovulon marker, however, has potential for women and couples trying to avoid pregnancy. Except for one of the cycles, the OL to O period ranged from 4 to 11 days with an average of 7.2 days. This length is somewhat longer than the average length of the total fertile period (6 days) as defined by the ovulation method. The long-term Ovulon predictive peak only had a modest correlation with the LH surge (r = 0.61) and with the peak in cervical mucus (r = 0.71). The conclusion is that at this time the OL is a very rough predictive marker of the beginning of the fertile period.
A limitation of the study is that the Ovulon was only tested on a small number of healthy women who had relatively regular menstrual cycles. Also, the Ovulon monitors were prototype instruments. For the Ovulon to be useful as a family planning method further testing will need to take place with women with varying cyclic patterns (eg, postpartum, breastfeeding, infertile, long cycles) and with refined instruments. Another limitation of the study is that the LH surge in the urine and the peak day of cervical mucus are indirect tests of ovulation. Use of serial transvaginal ultrasonography would add more precision and validity to the study. The expense of serial ultrasonography was beyond the scope and budget of this study. A final limitation of this study is that Ovulon data from 5 cycles (ie, in cycle number 3.2, 8.1, 8.2, 9.1, and 10.2) were interpreted in light of the peak in cervical mucus rather than by strict adherence to the established algorithm. These were cycles with Ovulon profiles that deviated from the expected or baseline pattern for reasons that are not understood. The expectation is that a larger study with a variety of reproductive categories with a range of clinical and biochemical measurements will provide that understanding.
Nurse-midwives and nurses have long incorporated teaching women about their body's physiology as part of educating women in self-care measures. Use of convenient, safe, and accurate devices to monitor physiologic process, such as a woman's fertility cycle, should be advocated. A benefit of the Ovulon monitor is that it is a reusable instrument, unlike the urine LH test kits that need to be purchased for each cycle. The Ovulon fertility monitor has potential to be a very useful device to assist nurse-midwives in fertility and infertility assessment, therapy, and family planning.
Notes
- Address correspondence to Richard J. Fehring, DNSc, RN, Associate Professor, Marquette University, College of Nursing, Emory T. Clark Hall, P.O. Box 1881, Milwaukee, WI 53201-1881.
- Richard J. Fehring is an associate professor of nursing at Marquette University and the research facilitator. Dr. Fehring received his master of science and doctoral degree in nursing science from The Catholic University of America in Washington, DC. He is a past president of the American Academy of Natural Family Planning (NFP) and a certified NFP practitioner and educator.
- William D. Schlaff is chief of reproductive endocrinology and vice-chair and associate professor of obstetrics and gynecology at the University of Colorado Health Sciences Center.
- This research project was supported in part by the Marquette University Regular Research Grant. Technical assistance was provided by Vaclav Kirsner, PhD, President and CEO of Conception Technology Inc.
References
- Fehring R. New technology in natural family planning. J Gynecol Neonat Nurs 1991;20:199-205.
- Albrecht B, Fernando R, Regas J, Betz G. A new method for predicting and confirming ovulation. Fertil Steril 1985;44:200-5.
- Fernando RS, Regas J, Betz G. Ovulation prediction and detection with the CUE ovulation predictor. Human Reprod 1988;3:419-24.
- Moreno JE, Weitzman G, Doody M, Gibbons W, Besch P, Goldzieher J. Temporal relation of ovulation to salivary and vaginal electrical resistance patterns: implications for natural family planning. Contraception 1988;38:407-18.
- Corson G, Ghazi D, Kemmann E. Home urinary luteinizing hormone immunoassay: clinical applications. Fertil Steril 1990;53: 591-601.
- Royston P. Identifying the fertile phase of the human menstrual cycle. Stat Med 1991;10:221-40.
- Corson SL. Self-prediction of ovulation using a urinary luteinizing hormone immunoassay: clinical applications. Fertil Steril 1986;31 SuppI 8:760-3.
- Seibel M. Luteinizing hormone and ovulation timing. J Reprod Med 1986;31 Suppl 8:754-9.
- Hilgers TW, Abraham GE, Cavanaugh D. The peak symptom and the estimated time of ovulation. Obstet Gynecol 1978;52:575-82.
- Fehring R. Methods used to self-predict ovulation: a comparative study. J Gynecol Neonat Nurs 1990;19:233-7.
- Hilgers TW. The ovulation method of natural family planning. Omaha (NE): Pope Paul VI Institute Press, 1992.
- Fehring R, Lawrence D, Philpot C. The use-effectiveness of the Creighton model ovulation method of natural family planning. J Gynecol Neonat Nurs 1994;23:303-9.
- Wilcox AJ, Weinberg CR, Baird DD. Timing of the probability of conception, survival of the pregnancy, and sex of the baby. N Engl J Med 1995;333:1517-21.
Appendix
Table 1
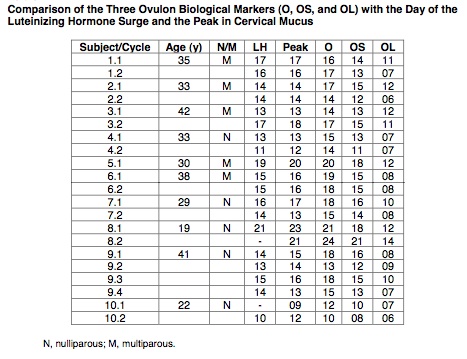
Figure 1
Figure 2
Article copyrights are held solely by author.
[ Japan-Lifeissues.net ] [ OMI Japan/Korea ]